Meet Dr. Kousa

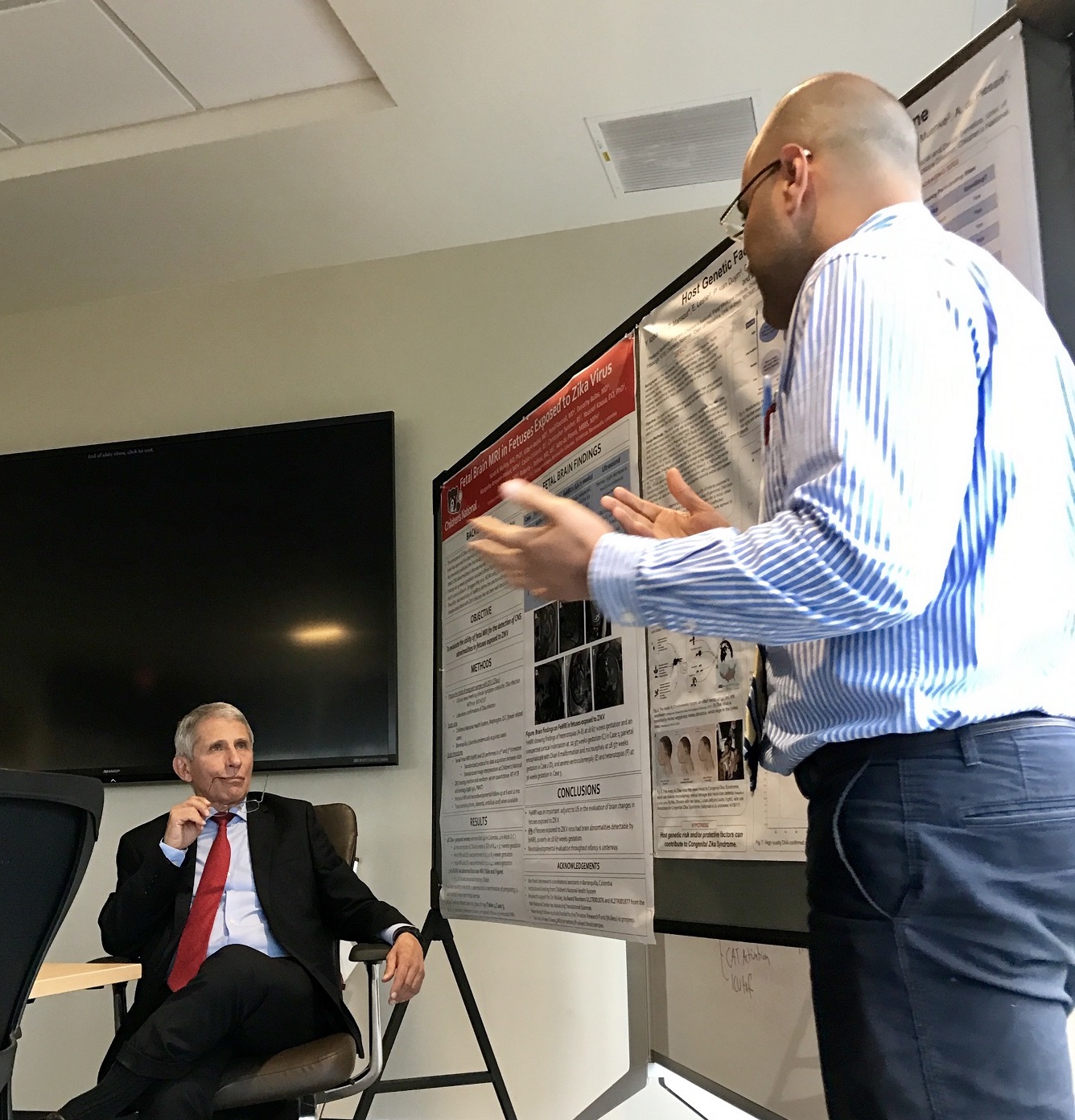
Youssef A. Kousa, M.S., D.O., Ph.D., is a physician-scientist specializing in neonatal neurology at Children’s National Hospital in Washington, D.C. During his pediatric internship, he founded an international, transdisciplinary research team, the Zika Genetics Consortium, to study the 2015 Zika virus pandemic and model human genetic modifiers in neuroinfectious diseases and neurodevelopmental disorders. Dr. Kousa completed a combined pediatrics and child neurology residency at Children’s National and the D.O.-Ph.D. Physician Scientist Training Program at Michigan State University. Dr. Kousa directs the Perinatal Neuroinfections Clinic at Children’s National and is an Instructor in Neurology, Pediatrics, & Genomics, and Precision Medicine at George Washington University School of Medicine, Washington, D.C.
Dr. Kousa’s interest in global health traces back to his early childhood in Alexandria, Egypt. One day, a seven-year-old Dr. Kousa accidentally kicked a soccer ball over a fence surrounding an empty lot where he was playing. While clambering over to retrieve the lost ball, his ankle was pierced by the razor sharp top of the metal paling. “I hung there for a second with my ankle caught and eventually was able to get off,” Dr. Kousa recalls. Without access to high quality care, Dr. Kousa’s family “threw some betadine” on his severely cut ankle and got on with it. Unfortunately, it became so infected Dr. Kousa almost lost the lower half of his leg.
In Egypt, Dr. Kousa explains, “pharmacists act as primary care physicians, so my mom took me to a pharmacist.” The pharmacist was alarmed at the severity of the infection and required that the young Dr. Kousa return to the pharmacy every other day for several weeks to make sure the infection improved. “I was lucky enough to have someone there to help me save my leg,” says Dr. Kousa, “in other cases where kids don’t have that access, they actually lose their legs.”
“There are lots of other examples around us everyday where we see someone who just wasn’t served by the healthcare system,” adds Dr. Kousa, “that could be due to a lack of personal, family, community, society, or state resources. I have this at the back of my mind all the time.” For Dr. Kousa, like the pharmacist who made sure his leg healed fully, “going above and beyond is what being a pediatrician is all about, saying ‘your problem is my problem’ and addressing it together. That is the attitude I bring to my patients here and abroad.” Dr. Kousa aims to help ameliorate illness and disease that result from lack of access to medical care. “What can we do to prevent this problem in future generations,” he asks, “what can we do to improve this for children to come?”
For Dr. Kousa, studying Zika presented a confluence of clinical, research, and personal priorities. Zika virus disproportionately affects low and middle income countries and families. Rates of transmission and infection correlate with indicators of poverty such as unhealthy housing, water access, and sanitation. Zika was also largely an academic gray area. “We didn’t understand how a mosquito borne virus could affect the mom, go through the placenta, get into the fetus and affect the fetal brain,” he adds. “There are no other examples of that in human beings having an epidemic and pandemic effect on human health.” At the time of the Zika outbreak in 2015-16, Dr. Kousa’s wife was pregnant with their first child. “That brought into sharp focus for me how communities and services can impact individual lives very significantly, directly, and differently,” he says. Dr. Kousa saw focusing on Zika as an opportunity to help prevent neurodevelopmental disabilities in children in low and high risk environments and a chance to better understand this class of neurodevelopmental disease and disorder.
In 2017, Dr. Kousa was granted an Explorations in Global Health Pilot Award from the Global Health Initiative at CN to study Zika. This project had the primary goal of supporting enrollment of and sample collections from mother-infant dyads exposed to Zika virus in Colombia. The data collected during this initial pilot award has served as the foundation for Dr. Kousa’s subsequent work in Zika research and the growth of the Zika Genetics Consortium.
“Zika was groundbreaking and a surprise to so many people in different fields,” recalls Dr. Kousa, “we needed to work together to understand it and work towards treatment.” The Consortium is designed to do just that. Bringing together the expertise of field leaders, it takes a transdisciplinary approach to disease prevention by integrating and leveraging team science, systems biology and genomics. Dr. Kousa serves as the Principal Investigator, overseeing six years of rapid growth. Since 2016, the Consortium has grown from 5 to 22 investigators and expanded from 4 initial sites to include projects at 17 separate sites in Brazil, Colombia, Puerto Rico, Guatemala, Nicaragua, and the international community here in DC. The Consortium regularly collaborates with 13 different institutions, and has secured commitments from the National Institutes of Health and Centers for Disease Control and Prevention which enabled expansion to 12 additional project sites.
The Consortium’s work is presently focused on establishing a robust genetic database to better understand Zika and its mechanism of disease by bringing together over 13,000 participants in the Western Hemisphere. The GHI Explorations Pilot Award “was one of the most important grants we received,” describes Dr. Kousa, “it allowed us to bring samples from Colombia, isolate DNA, and establish the framework for the rest of the project.” This framework enables the Consortium to collect data without the normal expense by collaborating with existing projects. “When you’re working in low resource settings and you’re a junior investigator,” Dr. Kousa adds, “you have to be creative and resourceful.”
Rather than dictating the kinds of samples and data each project site should collect, “we allowed each study site to contribute the samples and clinical data they thought were most important around a core set of standard metrics,” describes Dr. Kousa. “We proposed adding a genetic component to their existing study which was a marginal cost for them because they were already collecting the data,” Dr. Kousa explains. “For us the benefit was enormous because we were able to ramp up the clinical data collection without having to invest in independent sample collection.” By collaborating with existing studies, the Consortium has been able to collect significant amounts of data for comparably low cost and in a very short period of time. These local partner sites ship genetic samples to the Consortium at Children’s National where DNA can be isolated from these tissue samples and used to create a DNA bank through whole exome sequencing initially funded by the Explorations Award from GHI. “This data bank is used for all the work we are doing now,” describes Dr. Kousa.
The success of the initial project helped the group gain access to greater numbers of participants and samples. “That data established a framework and a pipeline for all the samples we are collecting,” says Dr. Kousa. The CDC and NIH both granted the Consortium access to multiple thousands of patient cohorts already enrolled in studies on Zika. This information is being added daily to the data bank established during the Explorations Pilot Award and has been used in several publications by the group. “We are actively working on 3,000 participant samples and will ultimately work through 13,000,” reports Dr. Kousa. Since the pilot funding, the group has received over 100,000 dollars in external support for their work and continues to apply for additional funding to expand this crucial resource for understanding and eventually preventing the neurodevelopmental effects of Zika virus.